- 782.91 KB
- 14页
- 1、本文档共5页,可阅读全部内容。
- 2、本文档内容版权归属内容提供方,所产生的收益全部归内容提供方所有。如果您对本文有版权争议,可选择认领,认领后既往收益都归您。
- 3、本文档由用户上传,本站不保证质量和数量令人满意,可能有诸多瑕疵,付费之前,请仔细先通过免费阅读内容等途径辨别内容交易风险。如存在严重挂羊头卖狗肉之情形,可联系本站下载客服投诉处理。
- 文档侵权举报电话:19940600175。
1AMERICANTHORACICSOCIETYDOCUMENTSAnOfficialAmericanThoracicSociety/EuropeanRespiratorySocietyPolicyStatement:EnhancingImplementation,Use,andDeliveryofPulmonaryRehabilitationCarolynL.Rochester,IoannisVogiatzis,AnneE.Holland,SuzanneC.Lareau,DarcyD.Marciniuk,MiloA.Puhan,MartijnA.Spruit,SarahMasefield,RichardCasaburi,EnricoM.Clini,RebeccaCrouch,JudithGarcia-Aymerich,ChrisGarvey,RogerS.Goldstein,KylieHill,MichaelMorgan,LindaNici,FabioPitta,AndrewL.Ries,SallyJ.Singh,ThierryTroosters,PeterJ.Wijkstra,BarbaraP.Yawn,andRichardL.ZuWallack;onbehalfoftheATS/ERSTaskForceonPolicyinPulmonaryRehabilitationTHISOFFICIALPOLICYSTATEMENTOFTHEAMERICANTHORACICSOCIETY(ATS)ANDTHEEUROPEANRESPIRATORYSOCIETY(ERS)WASAPPROVEDBYTHEATSBOARDOFDIRECTORS,OCTOBER2015,ANDBYTHEERSSCIENCECOUNCIL,SEPTEMBER2015Rationale:Pulmonaryrehabilitation(PR)hasdemonstratedreviewers.Aftercyclesofreviewandrevisions,thestatementwasphysiological,symptom-reducing,psychosocial,andhealthreviewedandformallyapprovedbytheBoardofDirectorsoftheATSeconomicbenefitsforpatientswithchronicrespiratorydiseases,yetitandtheScienceCouncilandExecutiveCommitteeoftheERS.isunderutilizedworldwide.Insufficientfunding,resources,andreimbursement;lackofhealthcareprofessional,payer,andpatientMainResults:Thisdocumentarticulatespolicyrecommendationsawarenessandknowledge;andadditionalpatient-relatedbarriersallforadvancinghealthcareprofessional,payer,andpatientawarenesscontributetothegapbetweentheknowledgeofthescienceandbenefitsandknowledgeofPR,increasingpatientaccesstoPR,andensuringofPRandtheactualdeliveryofPRservicestosuitablepatients.qualityofPRprograms.ItalsorecommendsareasoffutureresearchtoestablishevidencetosupportthedevelopmentofanupdatedObjectives:TheobjectivesofthisdocumentaretoenhancefundingandreimbursementpolicyregardingPR.implementation,use,anddeliveryofpulmonaryrehabilitationtosuitableindividualsworldwide.Conclusions:TheATSandERScommittoundertakeactionsthatwillimproveaccesstoanddeliveryofPRservicesforsuitablepatients.TheyMethods:MembersoftheAmericanThoracicSociety(ATS)callontheirmembersandotherhealthprofessionalsocieties,payers,PulmonaryRehabilitationAssemblyandtheEuropeanRespiratorypatients,andpatientadvocacygroupstojoininthiscommitment.Society(ERS)RehabilitationandChronicCareGroupestablishedaTaskForceandwritingcommitteetodevelopapolicystatementonKeywords:pulmonaryrehabilitation;policy;healthcare;chronicPR.Thedocumentwasmodifiedbasedonfeedbackfromexpertpeerrespiratorydiseases;accessContentsPatientAwarenessandLimitationsonPREligibilityOverviewKnowledgeBasedonCOPDDiseaseIntroductionIncreasingPatientAccesstoPRSeverityMethodsLackofAdequatePRLimitationsonPREligibilityoverBackground:PRInfrastructureandInadequateTimeIncreasingAwarenessandProgramCommissioningPatient-LevelBarrierstoPRKnowledgeofPRGeographicInaccessibilityLimitedNumberofPRHealthcareProfessionalImprovingAccesstoPRforHealthcareProfessionalsAwarenessandKnowledgePersonswithNon-COPDEnsuringQualityofPRProgramsPayerAwarenessandRespiratoryDisordersFutureResearchToAdvanceKnowledgeEvidence-basedPolicyinPRORCIDID:0000-0002-6343-6050(C.L.R.).Thisarticlehasanonlinesupplement,whichisaccessiblefromthisissuestableofcontentsatwww.atsjournals.orgAmJRespirCritCareMedVol192,Iss11,pp13731386,Dec1,2015Copyright©2015bytheAmericanThoracicSocietyDOI:10.1164/rccm.201510-1966STInternetaddress:www.atsjournals.orgAmericanThoracicSocietyDocuments1373guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSOverviewimplementation,use,anddeliveryofPRperformancemetricstoenablethatarediscussedinthisstatementincluderecommendationsforinternationalPulmonaryrehabilitation(PR)isathefollowing:standardsbasedonevidenceandbest“comprehensiveinterventionbasedonapractice.dPhysicianandalliedhealthcarethoroughpatientassessmentfollowedbydFurtherresearchshouldbeundertakenprofessionaltraineeswhotreatpatientspatient-tailoredtherapiesthatinclude,buttoadvanceevidence-basedpolicyinPR,withchronicrespiratorydiseasesshouldarenotlimitedto,exercisetraining,includingfurtherinvestigationregardinghaveformaltraininginthescience,education,andbehaviorchange,designedthecost-effectivenessofPRforchronicprocess,andbenefitsofPR.Trainingtoimprovethephysicalandpsychologicalrespiratorydisorders,innovativemodelsrequirementsshouldbespecifiedinconditionofpeoplewithchronicofPRdeliverythatwillimprovepatients’nationaltrainingcurriculumdocuments,accessanduptake,andthebarriersandrespiratorydiseaseandtopromotetheandconsistencyshouldbemaintainedinfacilitatorsofPRprogramreferral,long-termadherencetohealth-enhancingprogramsforeachhealthcaredisciplineaccessibility,enrollment,andadherence.behaviors”(1).PRreducespatients’andacrossdisciplines.symptoms;improveslimbmusclefunction,dPhysiciansandotherhealthcareexercisecapacity,emotionalfunction,professionalsinclinicalpracticeshouldIntroductionqualityoflife,knowledge,andself-efficacy;haveeducationalopportunitiesinthehashealtheconomicbenefits(1–12);andisprocessandbenefitsofPRconsistentPulmonaryrehabilitation(PR)hasanessentialcomponentoftheintegratedwithevidence-basedstatementsanddemonstratedphysiological,symptom-careofpatientswithchronicrespiratoryguidelines.reducing,psychosocial,andhealthdiseases.However,despiteitsclearbenefits,dToincreasepayerawarenessandeconomicbenefitsinmultipleoutcomeareasPRisgrosslyunderutilizedandisfrequentlyknowledgeofPR,healthcareforpatientswithchronicrespiratoryinaccessibletopatients.Insufficientprofessionalsandpatientadvocacydiseases(1–8,10–12,15–49).Assuch,itfunding;limitedresourcesforPRprograms;groupsshoulddevelopanddisseminateshouldbeastandardofcarealongsideotherinadequateallocationofhealthsysteminformationontheprocess,benefits,well-establishedtreatments(suchasreimbursementforPR;lackofhealthcarecosts,andcost-effectivenessofPRtopharmacotherapy,supplementaloxygen,orprofessional,payer,patient,andcaregiverpayers.noninvasiveventilation)forpatientswithaawarenessandknowledgeregardingthedToincreasepatientawarenessandchronicrespiratorydisease.Yet,PRprocessandbenefitsofPR;suboptimaluseknowledgeofPR,professionalsocietiesremainsgrosslyunderutilizedworldwideofPRbysuitablepatients(13,14);andandpatientadvocacyandeducation(15,50);itisfrequentlynotincludedinthelimitedtrainingopportunitiesforPRexpertsshouldcollaborateintheintegratedcareofpatientswithchronicprofessionalsallcontributetothegapdevelopmentoflanguage,education-respiratorydisordersandisoftenbetweenthescienceandbenefitsofPRlevel,andculturallyappropriateinaccessibletopatients.Indeed,a(1,11,15)andtheactualdeliveryofPReducationmaterialsinmultipleformatssubstantialgapexistsbetweenknowledgeservices.forpatientswithchronicrespiratoryregardingthescienceandbenefitsofPRDetailsofthescienceanddeliveryofPRdiseaseregardingtheprocessand(11,12,15)andtheactualdeliveryofPRwerehighlightedinthe2013AmericanbenefitsofPR.Communicationservices(15,50).ReasonsforthisgapThoracicSociety/EuropeanRespiratorycampaignsregardingPRshouldbeinclude:insufficientfunding;limitedSocietyStatementonPR(1).Thisnewaddressedtothegeneralpublic.resourcesforPRprograms;inadequatePolicyStatementhasadifferentfocus:itdPatientaccesstoPRshouldbeimprovedallocationofhealthsystemreimbursementprovidespolicyrecommendationswiththebyaugmentingprogramcommissioningforPR;lackofhealthcareprofessional,principalobjectiveofexpandingthethroughincreasedsustainablepayerpayer,patient,andcaregiverawarenessofprovisionofPRtosuitableindividualsfunding,creatingnewPRprogramsandknowledgeregardingtheprocessandworldwide.ItrepresentstheconsensusofingeographicareaswheredemandbenefitsofPR;suboptimaluseofPRbyinternationalexpertsinthefieldofPR,exceedscapacity,anddevelopingandsuitablepatients(13,14);andlimitedexpertsinprimarycare,andinternationalinvestigatingnovelPRprogrammodelstrainingopportunitiesforPRprofessionals.patientadvocates.Itprovidesthatwillmakeevidence-basedPRmoreTheseissuesappeartobeworldwideinrecommendationsthataddresskeyaccessibleandacceptabletopatientsandscope(15).Importantly,also,althoughprocessescentraltoachievingourobjectivespayers.SelectioncriteriaforPRshouldintensiveinpatientrehabilitationservicesofenhancingimplementation,use,andreflectcurrentpublishedevidence.forthesickestpatientsarewidelydeliveryofPR,includingincreasingdPRprogramsshouldfollowrelevantdistributed,availabilityofoutpatientorhealthcareprofessional,payer,andpatientevidence-basedclinicalguidelinesandcommunity-basedPRprogramsisawarenessandknowledgeofPR;increasingdemonstratethemeasurementofinsufficientorlackinginmanygeographicpatientaccesstoPR;andensuringqualitystandardoutcomestodocumentbenefits,areas.Moreover,withinandamongofPRprograms.Italsoprovidesquality,andsafety.countries,PRisheterogeneousregardingsuggestionsforactionableitemsthatwilldAcoresetofprocessesandoutcomesprogramstructure,content,staffing,fosterimplementationofthepolicyshouldbeestablishedtoenablenationalavailableresources,andpatientreferralrecommendations.NoteworthypolicyandinternationalbenchmarkinginPR;practices(15,50,51).Thisheterogeneityrecommendationstoincreasethisshouldincludebothprocessandhasthepotentialtocompoundtheissues1374AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSlistedaboveandtoadverselyaffecttheconsensusprocesswasfollowedtodevelopadvancesinthescienceanddeliveryofPRqualityofprograms.thispolicystatementbetweenMay2013werehighlightedinthe2013ATS/ERSPRThisAmericanThoracicSociety(ATS)/andJanuary2015.InformalsurveysStatement(1,12).TheestablishedbenefitsEuropeanRespiratorySociety(ERS)Policyprovidedinputfrompatients,patientofPRaresummarizedinTable1.Statementprovidespolicyrecommendationsadvocacygroups(includingtheATSPublicPRisbeneficialthroughoutthecoursewiththeprincipalobjectiveofexpandingAdvisoryRoundtableandELF),insuranceofdiseaseforsymptomaticmedicallytheprovisionofPRtosuitableindividuals.Topayers,aswellasprimarycareandPRstablepatientswithCOPD(75)andotherthisend,ourgoalsareto:healthcareproviders(seedetailsoftimelinechronicrespiratorydisorders(11),andandprocessinTableE1intheonlinesupervised,center-basedPRisalsoeffective1.Raisepublicandpoliticalawarenessofsupplement).ThispolicystatementwasduringorsoonafteracuteexacerbationsofthevalueandspecificbenefitsofPR,modifiedbasedonfeedbackfromexpertCOPD(76,77).ComprehensivePRhas2.Triggeractionbyhealthcaresystemstopeerreviewers.Aftercyclesofreviewandsimilarbenefitswhendeliveredininpatient,provideadequatefundingsupportforrevisions,thestatementwasreviewedandoutpatient,andcommunity-basedsettingsPRservicesandtoincludeprovisionofformallyapprovedbytheBoardof(7,10,78,79).Generally,aminimumofPRintheirstrategicplansforcareofDirectorsoftheATSandtheScience8weeks(twotothreesessionsperweek)ofrespiratorydiseases,CouncilandExecutiveCommitteeoftheoutpatientorcommunity-basedtreatment3.Increasehealthcareprofessionals’ERS.(orcomparablenumberofcontacthours)isprescriptionofPR,neededtoachieveaneffectonexercise4.EnhancedeliveryofPRthroughperformanceandqualityoflife(1,12,15,increasedprogramaccessandcapacity,Background:PR80);longerprogramsmayproducegreater5.Raiseawarenessofpatients’experiencesgains(12,80,81),andrepeatcoursesyieldandbarriersinaccessingandattendingPatientswithchronicrespiratorydiseasesbenefitsofequivalentmagnitudetothoseofPR,experiencedisablingsymptoms(includingfirst-timeparticipation(82).Exercise6.Engagepatientswithchronicrespiratorydyspneaandfatigue)andexercisetrainingisthecornerstonecomponentofdiseasesandtheircaregiverstointolerance,havelowphysicalactivityPR.Concurrentbehavioralinterventions,knowledgablyrequestaccesstoPR,levels,andreportimpairedqualityoflifesuchaspromotingself-efficacyand7.Facilitatethedevelopmentand(4,52–62).Thetremendousburdenposedteachingcollaborativeself-managementimplementationofqualitymetricsforbytheseissuesoftenpersistsdespiteskills,arealsointegraltooptimizingpatienttheinclusionofPRintotheintegratedoptimalpharmacologictreatment.outcomes(83,84).PatientsgraduatingcareofpatientswithachronicMoreover,personswithrespiratorydiseasesfromaPRprogramstandtobenefitfromarespiratorydisease,haveheterogeneousfeatures,and,formany,home,community-based,orprogram-8.Laythegroundworkfordevelopmentofextrapulmonarymanifestationssuchasbasedmaintenanceexerciseprogramtoaprocesstoimplementthepolicyskeletalmuscledysfunction(62–69)andsupportthecontinuationofpositiverecommendationsstatedinthismedicalandpsychologicalcomorbiditiesexercisebehavior(85).document.(suchasanxietyand/ordepression)arekeyKeyprocessescentraltoachievingthesecontributorstotheirsymptomsandobjectivesinclude:increasinghealthcarefunctionallimitations(70–73).PR,asprofessional,payer,andpatientawarenessdefinedinthe2013OfficialATS/ERSTable1.BenefitsofPulmonaryandknowledgeofPR;increasingpatientStatement,is“acomprehensiveRehabilitation(1–3,5,7,10–12,16–47,accesstoPR;andpromotingqualityPRinterventionbasedonathoroughpatient49,63,140,141)programs.Itisessentialthatprogramassessmentfollowedbypatient-tailoredqualitystandardsbemetwhilemaintainingtherapiesthatinclude,butarenotlimiteddReducedhospitalizationcostefficiencytoensureoptimalclinicalto,exercisetraining,education,anddReducedunscheduledhealthcarevisitsoutcomesforpatientsaswellassustainablebehaviorchange,designedtoimprovethedImprovedexercisecapacityfundingofPRprograms.physicalandpsychologicalconditionofdReducedsymptomsofdyspneaandlegpeoplewithchronicrespiratorydiseaseanddiscomforttopromotethelong-termadherencetodImprovedlimbmusclestrengthandMethodsendurancehealth-enhancingbehaviors”(1,12).ItdImprovedhealth-relatedqualityoflifeemphasizesstabilizationand/orreversalofdImprovedfunctionalcapacity(e.g.,AnadhocTaskForcewasformed,extrapulmonarymanifestationsandactivitiesofdailyliving)composedofexpertsfromtheATScomorbiditiesofchronicrespiratorydiseasedImprovedemotionalfunctiondEnhancedself-efficacyandknowledgePulmonaryRehabilitationAssembly,theaswellastheimportanceofbehaviordEnhancedcollaborativeERSRehabilitationandChronicCarechange.PRisanessentialcomponentofanself-managementGroup,theATSandERSDocumentsintegratedcontinuumofhealthcareacrossdPotentialforincreaseddailyphysicalDevelopmentandImplementationthetrajectoryofthepatient’sillnessaswellactivitylevelsCommittees,representativesfromtheasacrosshealthcareprovidersandvenues.Note:theorderanddegreeofevidenceforeachEuropeanLungFoundation(ELF),andItisnotanewtherapy;thefirstofficialATSoftheabove-notedbenefitsvariesamongprimarycarerepresentativesfromtheconsensusstatementonitsapplicationwaschronicobstructivepulmonarydiseaseandotherUnitedStatesandEurope.Aniterativepublishedin1981(74).Majorrecentrespiratorydiseases(9,11).AmericanThoracicSocietyDocuments1375guide.medlive.cn
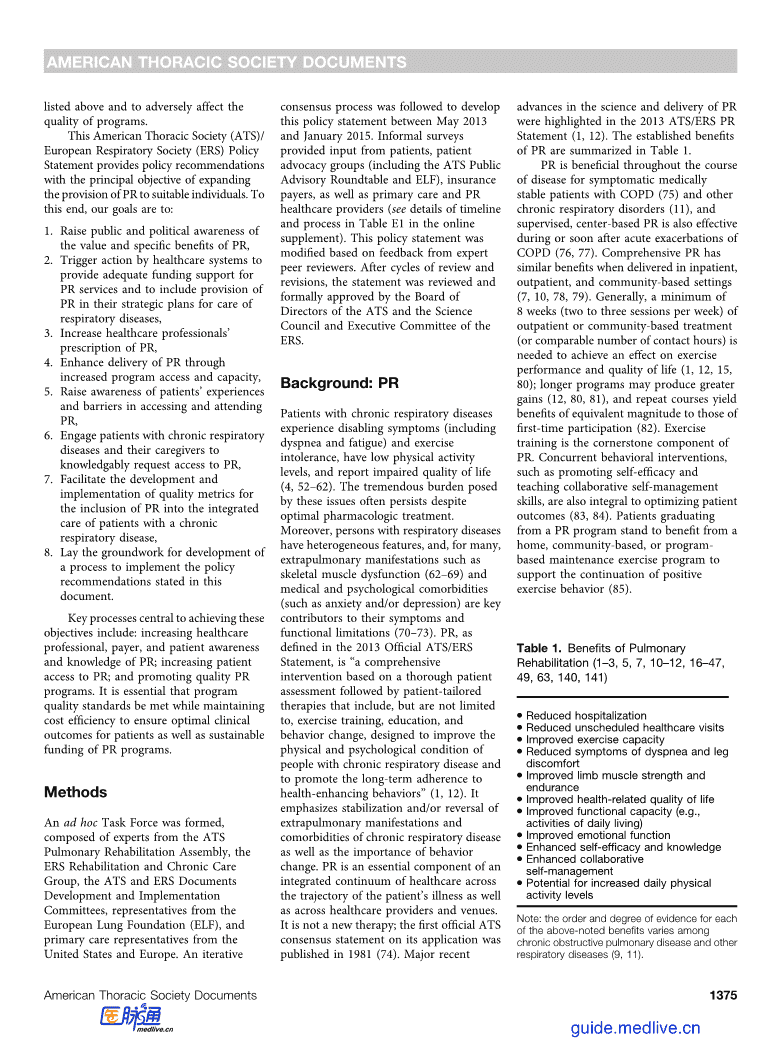
AMERICANTHORACICSOCIETYDOCUMENTSTable2.ExamplesofTrainingawarenessofPRiscurrentlyabarriertoincreasinghealthcareprofessionalOpportunitiesinPulmonaryRehabilitationpatientreferral(86).awarenessandknowledgeofPRareforHealthcareProfessionalsHealthcaretrainees.AwarenessofPRprovidedinBoxes1and2.shouldideallybeginduringtraining.Currently,exposuretotheprocesses,PayerAwarenessandKnowledgedERSHERMESprogramindications,andbenefitsofPRaregenerallyPRisoneofthemostcost-effectivedATSandERSpostgraduatecoursesonPR(heldperiodicallyatannualinternationalnotamandatorypartoftheeducationoftreatmentinterventionsavailableforconferences)physicians,nursepractitioners,physicianpatientswithchronicrespiratorydiseasesdAmericanCollegeofChestPhysiciansassociates,oralliedhealthcareprofessionals.(93–97)andisassociatedwithasubstantialAnnualConferenceandspecialtyboardAlthoughdetailedrecommendationsforreductioninhospitalizations,otherurgentreviewmaterialstraininginPRexistinsomecountries,suchhealthcareresourceuse,andhealthcaredLungFoundationAustraliaPRtrainingOnlineastheUK(87),evenforpulmonarycosts(76,93–95,98,99).Forexample,itsdLocalcoursesinseveralcountries(e.g.,physicians,statedtrainingrequirementsarevalueissituatedfavorablywithinthetheUK,theNetherlands)oftenvagueorlimited.ThisistrueinthecontextofothercomponentsoftherapyfordCoursesonPRpromotedbyrespiratoryUnitedStates(88),Canada(89),theCOPDintheUK(Figure1)(96,97);thesocietiesinLatinAmericaNetherlands(90),Australia(91),andLatinrelativevaluecostsarenotyetstudiedDefinitionofabbreviations:ATS=AmericanAmerica(92).Furthermore,primarycareinnon-COPDchronicrespiratoryThoracicSociety;ERS=EuropeanRespiratoryandotherhealthcareprofessionals,whodisorders.Nevertheless,payerawarenessofSociety;HERMES=HarmonisedEducationinprovidecareforthemajorityofpatientsPRisoftenpoor,andfundingofPRisRespiratoryMedicineforEuropeanSpecialists;withrespiratorydisease,oftenhaveveryinadequate.AdequatefundingisvitaltoPRPR=pulmonaryrehabilitation.LungFoundationAustraliatrainingonlinecanbelittleifanyexposuretoPRinthecourseofprogramavailability,capacity,effectiveness,foundathttp://lungfoundation.com.au/theirtraining.Somepostgraduatetrainingandviability.Althoughheterogeneoushealth-professionals/training-and-education/isavailable(Table2),butitisnotpaymentstructuresandresourcesexistpulmonary-rehabilitation-training-online/.mandatory,isoftennotstandardized,andiswithinandacrosscountries(15),increasingHERMESeducationinRespiratoryMedicineprogramoftheERScanbefoundatatthediscretionofthehealthcarepayerknowledgeisthefirststeptowardhttp://hermes.ersnet.org.professional.Thereisaclearneedforsecuringadequatelong-termfunding.enhancedandmorestandardizedexposureInformaldiscussionswithrepresentativestoPRwithinexistinghealthcarefromgovernmentandprivateinsuranceIncreasingAwarenessandprofessionals’trainingprograms.payersinseveralcontinentsaspartofKnowledgeofPRHealthcareprofessionalsinclinicaldevelopmentofthisdocumentsuggestedtheirpractice.ThereisaneedformoreperceptionthatcurrentfundingandHealthcareProfessionalAwarenesseducationandlearningopportunitiesforreimbursementforPRareadequate.However,andKnowledgeestablishedpracticingprimaryandtheexistenceofpayer-relatedbarriersisPatientswillnotreceivePRunlesstheyarespecialtycarephysicians,nursesupportedbyapublishedsurveyinthereferred,whichisunlikelytooccurunlesspractitioners,physicianassociates,andUK(93)andbyaninformalsurveyhealthcareprofessionals(includingprimaryotheralliedhealthcareprofessionalsconductedbymembersoftheTaskForceforcareandspecialistphysicians,nurseabouttheprocessandbenefitsofPR.thisdocument(TableE2).Thesesurveyspractitioners,physicianassociates,andIncreasedknowledgeofPRcouldfosterpointtoaninadequateappreciationamongalliedhealthprofessionals)areawareofthedialoguebetweenhealthcareprofessionalspayersoftheclinicaleffectivenessandexistenceofPRandhaveknowledgeofitsandtheirpatients,therebypromotingcost-effectivenessofPR.Tothisend,benefits.SuboptimalhealthcareprofessionalreferralstoPR.RecommendationsforincreaseddialogueandeffectiveBox1:IncreasingHealthcareProfessionalTraineeAwarenessandKnowledgeofPRRecommendations:dPhysicianandalliedhealthcareprofessionaltraineeswhotreatpatientswithchronicrespiratorydiseasesshouldhavecoreformaltraininginPR,includingitsscientificrationale,process,andbenefits.ThisincludesuseoftrainingmodulescoveringthetopicsshowninTable3andprovisionofpractical“hands-on”experiences.dTrainingrequirementsshouldbespecifiedinnationaltrainingcurriculumdocuments,andconsistencyshouldbemaintainedinprogramsforeachhealthcaredisciplineandacrossdisciplines.ActionableItems:dEducationalauthoritiesfromrespiratory,primarycare,nursing,andotheralliedhealthcareprofessionals’societiescollaboratetodevelopspecificcurriculaforPRtrainingfortheirrespectivehealthcaretrainees.dRespiratory,primarycare,andalliedhealthcareprofessionals’societiesestablishnationaltrainingprogramcurricularregistriestocoordinateandmonitorprogresstowardcurriculadevelopment.1376AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSTable3.TopicsforInclusioninEducationalMaterialsforHealthcareBox2:IncreasingAwarenessandKnowledgeofPRamongProfessionalsHealthcareProfessionalsinClinicalPracticeRecommendation:dThescientificrationaleforPRdPhysiciansandotherhealthcareprofessionalsinclinicalpracticeshouldhavedEstablishedbenefitsofPReducationalopportunitiesintheprocessandbenefitsofPRconsistentwithdComponentsofamultidisciplinaryPRprogramevidence-basedstatementsandguidelines.dSelectionandreferralofappropriatepatients,includingpersonswithActionableItems:non-COPDrespiratorydisordersdPrimarycare,specialtyphysician,andalliedhealthprofessionalsocietiespartnerdPatientassessmentandoutcomesmeasurementtechniqueswithexpertsinPRtodevelopandimplementmoreevidence-based,multiformatdProgramdesignanddeliveryinthecontextpostgraduateeducationalprogramsontheprocess,benefits,anduseofPR.oflocal/regionalresourcesdRespiratorysocietiesandnationalhealthauthoritiesprovidepracticaleducationaldRoleofPRintheintegratedcareofmaterialsforclinicians(coveringtopicsshowninTable3)andacontactlistoflocalpatientswithchronicrespiratoryPRprogramsintheclinicsetting.diseasesdImportanceofpatients’long-termdIncludePRinrelevantprofessionallearningofferings,suchasscientificmeetingsadherencetohealth-enhancingandcontinuingmedicaleducationcourses.behaviors(suchasphysicalactivity,dHealthcareprofessionalsdocumentthatPRwasofferedtosuitablepatientsinimmunizations,abstinencefromclinicalsettings(includingspecificationofthereasonsfornonreferral)asareflectionsmoking)afterPR:roleofhomecaregiversandimportanceofofawarenessandknowledgeofitsindicationsandbenefitsandtosupportqualitycoordinatedcarebetweenhealthcaremetricassessment.professionalsdIncorporate“clinicalreminderalerts”forPRreferralinelectronicmedicalrecorddOpportunitiesforadvancedcareplanningsystems.inthecontextofPRdRelevantlocal,regionalornationalinformationregardingfundingandpayerreimbursementforPRawarenessandknowledgeofPRareprovidedofPRasastandardofcareandtodCurrentgapsinaccess,barrierstopatientinBox3.distinguishPRfromchestphysiotherapy.participationinPRandpotentialIncreasingtheawarenessofPRamongthesolutionstotheseproblemsPatientAwarenessandKnowledgegeneralpublicisalsoessential.Relatives,Definitionofabbreviations:COPD=chronicPatientuptakeofPRandadherencetofriends,neighbors,coworkers,andothersobstructivepulmonarydisease;PR=pulmonaryparticipationinPRarestrikinglylowcanencouragepatientstoseekoutandrehabilitation.(5,13–15,41,50,100).MuchoftheparticipateinPR.PublicawarenessofPRresponsibilityfornonreferraltoPRrestsonmaybeenhancedthroughcommunicationcommunicationareneededbetweenPRhealthcareprofessionals(7),butinsufficientcampaigns,includingsocialmediaexpertsandproviders,healthcarepublicawarenessandknowledgeoftheplatforms(suchasFacebookandprofessionals,professionalsocieties(e.g.,ATS,processandhealthbenefitsofPR(14,41)YouTube).ItisimperativethatpatientsERS,andothers),payers,andhealthpolicyalsopreventpatientsfromseekingreferralidentifiedbyevidence-basedclinicalauthoritiesregardingtheestablishedbenefitstoandcompletionofaPRprogram.managementguidelinesashavingpotentialandcost-effectivenessofPRaswellastheProfessionalsocietiesandpatientadvocacytobenefitfromPRaremadeawareofthisprioritiesandconcernsofpayers.groupscanaugmenteffortstodisseminatetherapysothattheycanadvocateforaccessRecommendationsforincreasingpayerinformationandfacilitatepatientawarenesstoitthroughtheirregionalandnationalBox3:IncreasingPayerAwarenessandKnowledgeofPRRecommendations:dHealthcareprofessionalsandpatientadvocacygroupsshoulddevelopanddisseminateinformationonthecostsandcost-effectivenessofPRtopayers.dTheprocessandoutcomesofPRshouldbemademoretransparenttopayersbyPRserviceproviders.dHealthcareprofessionalsshouldinvestigatethecost-effectivenessofPRincountrieswhereinthisinformationislacking.ActionableItems:RespiratorydiseasesocietiesandPRproviders,incollaborationwithprimarycarehealthprofessionalgroupsandpatientadvocacygroups:BDevelopmethodsofdetailingthebenefits,costs,andvalueofPRtobecommunicatedtopayers.BEnhanceplatformsandassureincreasedresourcesforcommunicatingtheeffectivenessofPRtopayers.BDevelopacoordinatedadvocacystrategytofacilitateincorporationofPRintohealthcaresystemsandpracticesasa“standardofcare”componentoftheoverallintegratedcareofpatientswithchronicrespiratorydiseases.AmericanThoracicSocietyDocuments1377guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSexceedsthecapacityofexistingprograms(4,15).CapacitycanbeincreasedbycreatingTelehealthforchronicnewprogramsand/orbyexpandingexistingdisease£92,000/QALY*programs.Bothapproacheswillrequiresignificantbuy-in,systemchange,andTripleTherapy£7,000–£187,000/QALYinvestmentfromhealthcareprofessionals,healthcarepolicy-makers,administrators,LABAandpayers.Thisshouldbefacilitatedby£8,000/QALYdemonstratingdatashowingreturnoninvestmentforthelocalhealthcaresystem4C/FPOTiotropiumandbyprovidingpolicyadvicefor£7,000/QALYgovernmentsandnongovernmentalorganizationswhoadvocateforpeoplewithPulmonaryRehabilitationchronicdisease.EstablishmentofnewPR£2,000–8,000/QALYprogramsandstrategiestoincreasethecapacityofexistingPRprogramsmustStopSmokingSupportwithpharmacotherapy£2,000/QALYfollowrecommendationsasdetailedintheATS/ERSPRStatement(1,12)andotherPRguidelines(3,5,7,10).ThisincludesFluvaccination£1,000/QALYin“atrisk”populationadequateinfrastructure(spaceforphysicalconditioning,exercisetraining,andFigure1.Cost-effectivenessofpulmonaryrehabilitationrelativetoothertreatmentsforchronicmonitoringequipment;resourcesforobstructivepulmonarydisease.ReprintedfromReference96.*Costperquality-adjustedlifeyearequipmentmaintenanceandreplacement;(QALY).LABA=long-actingb-agonist.andspaceandresourcesforpatientassessmentandeducation),andstaffingadvocacyrepresentatives.inadequatePRservicestomeetpatientneeds.(number,training,experience,andRecommendationsforincreasingpatientThisshortfallinPRserviceaccessibilityandcompetency[101]).TheefficiencyofawarenessandknowledgeofPRarecapacityresultsfromseveralfactorsprogramsalsoimpactscapacity.providedinBox4.consideredbelow.Measuringprocessmetrics(suchastimefrompatientreferraltoprogramuptake,IncreasingPatientAccessanduseofacentralplanningtoPRLackofAdequatePRInfrastructureadministrativestructureforpatientandInadequateProgramenrollment)isimportantinthisregard.VariableaccesstoPRcreatesCommissioningExpandingtherangeofprogrammodelsunacceptabledisparitiesinquality,evidence-DespitethehighvalueofPR(96),thedeliveredwithinexistingcomprehensivePRbasedhealthcare.Currently,therearenumberofpotentiallysuitablepatientsfarsettings(e.g.,outpatientorcommunitybased),Box4:IncreasingPatientAwarenessandKnowledgeofPRRecommendations:dProfessionalsocietiesandpatientadvocacyandeducationexpertsshouldcollaborateinthedevelopmentoflanguage,educationlevel,andculturallyappropriateeducationmaterialsinmultipleformats(e.g.,written,internetbased)forpatientswithchronicrespiratorydiseases,toenablethemtoknowledgeablyadvocateforaccesstoPR.dHealthcareprofessionalsshouldprovideinformationregardingtheprocessandbenefitsofPRtosuitablepatients.dCommunicationcampaignsshouldbeaddressedtothegeneralpublicregardingtheprocessandbenefitsofPR.ActionableItems:dProfessionalsocietiessuchastheATS,ERS,andotherspartnerwithnationalandinternationalpatientadvocacygroupstoprepareanddisseminatePR-relatededucationalmaterialsculturallyadaptedtoeachcountryandcompatiblewithpatienthealthliteracy,andtoensurethateducationalmessagesareconsistentinthematerialsforhealthcareprofessionals,patients,andfamilies.dProfessionalsocietiessuchastheATSandERSandpatientadvocacygroupsdisseminatetheabove-notededucationalmaterialstohospitals,clinics,communitycenters,andpatientsupportgroupsandmakethemavailableonline.dDevelopmediacampaignswithgovernmentalandprofessionalsocieties’supporttoincreasetheawarenessofpatientsandthegeneralpublicregardingthebenefitsofPR,exercise,andphysicalactivity.dPRproviderswithinprofessionalsocietiessuchasATSandERSadvocatethatpharmaceuticalcompanieswithaccesstopatientsspreadawarenessoftheexistenceandbenefitsofPRincombinationwithothertherapies(includingpharmacotherapyandsupplementaloxygen).1378AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSaddingPRasatreatmentoptionbebasedonsymptomsandfunctionalPatient-LevelBarrierstoPRwithinexistingcardiacorgeneralstatuslimitationratherthansolelyonthePatientsreferredtoPRconsistentlyreportrehabilitationprograms,oraddingadditionalseverityoflungfunctionimpairmentbarrierstoinitiationofandadherencewiththeessentialcomponentsofPR(besidesexercise(1–3,6,10,12).PReffectivelyaddressesintervention(13,14),anduptohalfofeligibletrainingthatconstitutesthecornerstoneofseveralissuesalsoexperiencedbypatientsreferredtoPRneverattend(14).IneveryPRprogram),suchasself-managementpersonswithmildtomoderateCOPD,additiontotravelandtransportationissues,trainingandpatienteducation,toincludingexertionaldyspnea(105–108),lackofsupportfromfamilymembersorinterventionscomposedsolelyofexercisedynamichyperinflation(107,108),othercaregivers,depression,comorbidillness,trainingcouldalsoincreaseprogramcapacityskeletalmuscledysfunction(63,107,anddisruptionofdailyroutineareandpatientaccesstoPR.Asignificant109),lowphysicalactivitylevels(110,particularlyimportant(14).MembersoftheincreaseinfundingsupportforPRwillbe111),depression(112),riskandimpactTaskForceforthisPolicyStatementalsoneededtoaddresseachoftheseissues.ofcomorbiditiessuchascardiovascularconductedaninformalsurveyofpatients’disease(113),exacerbationsofCOPDopinionsregardingaccesstoPRamongGeographicInaccessibility(114),andimpairedqualityoflife(115)membersofATS’PublicAdvisoryRoundtable,ELF’spatientorganizationWorldwide,accesstoPRislimitedin(Table1)(12).However,insomenetwork,theCOPDFoundation,andthemanygeographicareas,andinsomejurisdictions,accesstoPRislimitedbyPulmonaryFibrosisFoundation.ResponsescountriesPRprogramsarelackingregulationsspecifyinginsurancefrompatientswithawidevarietyofchronicaltogether(15,102).PatientscoverageofPRonlyforstablepatientsrespiratoryconditionswereincluded.KeyfrequentlycitedistanceandlackofwithCOPDwhohavemoderatetoseverepatient-identifiedbarrierstoaccessingPRtransportationasamajorreasonforpoorairflowobstruction.Suchpoliciesarenotidentifiedinasurveyof1,686respondentsprogramuptakeoradherence(14).Itisinlinewithstrongevidencefromfrom29countries(FigureE1)included(inknownthattraveltimegreaterthan30randomizedtrialsthatshowthatbothdescendingorderoffrequency)lackofminutesisabarriertopatientpatientswithunstableCOPDwhostartawarenessofPR(“neverheardofit”),participationinPR(103).ThesefactorsrehabilitationduringorafteraninsufficientinformationonprocessorshouldbeconsideredwhennewPRexacerbations(76)andpatientswithpotentialefficacy,lackofavailablePRprogramsareestablished.stablemildtomoderateCOPDbenefitservices,andlackofinsurancecoverage.Thefromrehabilitation(116–118).findingsofthispatientsurveycorroborateImprovingAccesstoPRforPersonstheissuesregardingawarenessandwithNon-COPDRespiratoryLimitationsonPREligibilityoverTimeknowledgeofPRandaccesstoPRdiscussedDisordersThebenefitsof8to12weeksofPRtypicallyabove.Importantly,manyofthesebarriersPRhasdemonstratedeffectivenessforlastupto12months(17,21,119).Yet,seemmodifiablewithorchestratedactions.severalrespiratoryconditionsotherthanpatientslivewiththeirchronicrespiratoryCOPD(2,11).Randomizedcontrolledtrialsdiseasesoverthecourseoftheirlifetime.LimitedNumberofPRHealthcaredemonstratingitsbeneficialeffectsonProfessionalsexercisecapacity,symptoms,and/orhealth-EmphasisisplacedinPRprogramsonTrainedPRhealthcareprofessionalsarerelatedqualityoflifeareavailableinhealth-enhancingbehaviorchangeforthisnecessaryforprovisionofPRtopatients.interstitiallungdisease,bronchiectasis,reason.Nevertheless,anihilisticviewAvailabilityofeducation,training,andasthma,cysticfibrosis,lungtransplantation,towardPRisoftentakenbypayersandfundingforhealthcareprofessionalswholungcancer,andpulmonaryhypertensionhealthcareprofessionalsasaresultofastrivetobecomePRprovidersvarieswithin(16–30,32–34,36,38–40,42,43,45,46,potentiallylimiteddurationofthebenefitsandacrosscountries.Althoughformal104).Theremaybespecialconsiderationsresultingfrompatients’participationinadocumentationislacking,insufficientandadditionaltrainingforPRstaffsinglePRprogramcourse.InsomeavailabilityofPRprovidershasthepotentialrequiredwhenincludingpersonswithnon-countries(e.g.,theUnitedStates),thereisatolimitpatientaccesstoPR.COPDdisorders(3,11,12).PayerpayerlimitonthetotalnumberofPRRecommendationsforincreasingpatientreimbursementofPRfornon-COPDsessionspatientscanattend.ThisisaccesstoPRareprovidedinBox5.disordersremainslimitedinsomecounterproductive,becauserepeatcoursescountries.PayersandhealthcareofPRaffordsimilarbenefitstothoseofprofessionalsrequireknowledgeregardinginitialpatientparticipation(82)and,atEnsuringQualityofPRappropriatepatientselectioncriterialeastforCOPD,PRiseffectiveafteracuteProgramsaccordingtopublishedevidence.diseaseexacerbations(76,120),whichareassociatedwithworsenedsymptoms,ThequalityofPRprogramsisreflectedinLimitationsonPREligibilityBasedonfunctionaldecline,andhighhealthcareprocessandperformancemetrics.The2013COPDDiseaseSeveritycosts(121–123).Increasingpatients’accessATS/ERSPRStatement,the2013BritishAlthoughPRbenefitspersonswithmanytoPR,includingrepeatedcourseswhereThoracicSocietyqualitystandards,andrespiratorydisorders,muchoftheclinicallyindicated,hasthepotentialtootherdocuments(1,3,6,10,12,93,116,publishedliteraturehas,historically,improvepatients’healthoverthecourseof117)summarizetheevidenceunderpinningcenteredonCOPD.ProvisionofPRtheirlivesandtoreducehealthcareusebestpracticeforPR.ProgramcertificationservicesforpersonswithCOPDshouldcosts.isameansofensuringstandardsaremet.AmericanThoracicSocietyDocuments1379guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSBox5:IncreasingPatientAccesstoPRRecommendations:dPatientaccesstoPRshouldbeimprovedbyaugmentingprogramcommissioningthroughincreasedsustainablepayerfunding.dNewPRprogramsshouldbecreatedingeographicareaswheredemandexceedscapacity.dNovelPRprogrammodelsshouldbedevelopedandstudiedthatwillmakeevidence-basedPRmoreaccessibleandacceptabletopatientsandpayers;thismayincludenewapproacheswithinhospital-basedprograms,community-basedprograms,comprehensiveandwell-resourcedhome-basedortelehealth-supportedprograms,orothernovelmodelsofprogramdelivery.dSelectioncriteriaforPRshouldreflectcurrentpublishedevidence.TheevidenceindicatesthatpatientswhobenefitfromPRincludenotonlypersonswithmoderatetosevereairflowlimitationbutalsothosewithmildtomoderateairflowlimitationwithsymptom-limitedexercisetolerance,thoseafterhospitalizationforCOPDexacerbation,andthosewithsymptomaticnon-COPDrespiratoryconditions.Increasingpatientaccessforthesepatientgroupswilldependonincreasedreferrals,increasedpayerfunding,andpatientdemandforservices.ActionableItems:dPRproviderssystematicallydetailanddocumentthecostsofprovidingcomprehensivequalityPRservicesandsharethisinformationwiththoseadvocatingPRpolicies’reimbursementratetofacilitateappropriateandnecessaryreimbursement.dIdentifythenumberofpatientspotentiallysuitableforPR(basedonoutpatientandhospitaldischargedatabases)withinlocalandregionaljurisdictionstoassesstheneedforestablishmentofnewPRprogramsand/orincreasedcapacityofexistingprograms.dPRproviders,localfundingagencies,healthsystems,patients,andresearcherscollaboratetoestablishtheoptimalmodelsthatwillincreasePRcapacityanduptake.dProfessionalsocieties(suchasATS,ERS,andothers)auditexistingpatientselectioncriteriaforPRandworkwithaccreditationorganizationstobroadenpatientcandidacytoincludethosewithsymptomaticnon-COPDrespiratoryconditions,thoseafterhospitalizationforCOPDexacerbation,andsymptomaticpatientswithmildtomoderateairflowlimitation.dProfessionalrespiratorysocieties(suchasATS,ERS,andothers)audittheavailabilityofPRprovidersandtrainingprogramsforhealthcareprofessionalswhostrivetobecomePRproviders.dPatientsandtheirfamiliespartnerwithhealthcareprofessionals,advocacygroups,andhealthprofessionalsocietiestopetitionforgreatercapacityandaccesstoPRintermsofthenumbersofprograms,patienteligibility,andinsurancecoverage.dPRprogramsidentifylocalbarrierstopatientuptakeandadherencetoPRandoutlinestrategiestoaddressthesebarriers.dPayersofferincentivesforsuitablepatientstoparticipateinPR.dPayerslinkhealthcareprofessionals’patientreferralstoPRto“payforperformance.”Currently,onlytheAmericanAssociationpreparedtoworkcloselywithotherindividualizedrehabilitationaccordingtoofCardiovascularandPulmonaryhealthcareprofessionalstohandlethemulti-eachpatient’sneeds.ToassessprogramRehabilitation(intheUnitedStates)(2)morbiditypresentamongpersonsreferredforquality,clinicaloutcomesmustbeandsomecountriesinEurope(124)offerPR,includingthepsychologicalimpactandmeasuredforindividualpatientsandthiscertificationprocess.Implementationmanifestationsofchronicrespiratorydisease.presentedinaggregate.EssentialoutcomesofasimilarinternationallyrelevantprocessTobeuniversallyapplicable,theseprogrammeasurementsinPRinclude,atathatevaluatesPRprogramqualityandcomponentsmustbeimplementedwithminimum,thestandardizedassessmentofrewardsqualityprogramsisneeded.Thisconsiderationoflocalresources,aswellaspatients’functionalexercisecapacity,wouldfacilitatehighlightingandcultural,economic,andhealthcaresystemdyspnea,andhealthstatus(1–3,6,10,12).disseminationofqualitystandardsforPRdifferencesacrosscountries.ThehealthSeveraldisease-relevantmethodsareprogramstohealthcarefacilities,healthcareeconomicbenefitsofPRcanpotentiallybeavailableformeasuringtheseoutcomesprofessionals,andpolicymakers.furtherenhancedbyusingtheprogramasa(11,12).AssessmentofadditionalToqualifyasPR,programsmustinclude,vehicletopromoteincreaseddailyphysicalmultidimensionaloutcomes(consideredataminimum:astructuredandsupervisedactivity,whichmayinturnreducetheriskoffurtherinthe2013ATS/ERSStatementonexerciseprogramforpatientswithavarietyofhospitaladmission(129).PulmonaryRehabilitation)(1),includingrespiratoryconditions,apatienteducation/ThequalityofPRprogramsis(butnotlimitedto)impactofPRonbehavioralprogramintendedtofosterhealth-demonstratedbytheirsuccessinimprovingpsychologicalcomorbidityandmeasuresofenhancingbehavior,patientassessmentandpatientoutcomes.PatientsenteringPRthepatientexperience,isdesirable,becauseoutcomesmeasures,andprovisionofprogramsareheterogeneousregardingpatients’responsestoPRarerecommendationsforhome-basedexercisediseasestate,symptoms,functionalmultidimensional(130).Theselectionandandphysicalactivity(1,3,5,7,10,12,93,limitations,medicalcomorbidities,andstandardizationofoutcomemeasuresfor125–128).StaffofPRprogramsmusthavepsychologicburdenofdisease.PatientthepurposeofprogramcomparisonanddemonstratedcompetenciesinprovisionofassessmentsconductedatthestartofPRbenchmarkingwillvaryamongdifferentPR(101).Theymustalsobeawareofandbecharacterizepatientstoenabledeliveryofjurisdictions,butshouldbeguidedbythe1380AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSBox6:EnsuringQualityofPRProgramsRecommendations:dPRprogramsshouldfollowrelevantevidence-basedclinicalguidelinesanddemonstratethemeasurementofstandardoutcomes,todocumentbenefits,quality,andsafety.dAcoresetofprocessesandoutcomesshouldbeestablishedtoenablenationalandinternationalbenchmarkinginPR;thisshouldincludebothprocessandperformancemetricstoenablerecommendationsforinternationalstandardsbasedonevidenceandbestpractice.dPRprogramsshouldencourageandfosterpatients’long-termadherencetohealth-enhancingbehaviorstooptimizepatientwellnessandreducehealthcarecosts.ActionableItems:dNationalrespiratorysocietiesdevelopkeyperformanceandprocessindicatorstoassistintheprocessofprogramaccreditation.dIndividualPRprogramsdeveloppatientregistriesforpurposesofmonitoringprogramqualityandoutcomes.dPRprogramsfollowevidence-basedclinicalguidelines,includingprocess,outcomes,quality,andsafety,tojustifyreimbursementfrompayers.dPRprofessionalswithinprofessionalsocieties(suchasATSandERS)collaboratetomodifyandexpandexistingnationalPRregistriesforinternationaluse.respiratoryscientificcommunitybasedonforPRshouldbeconsistentacrossprograms,overthelongtermareessential.disease-relevantpublishedevidence.butsolutionstoachievethesestandardsmustInvolvementofhomecaregiversandcloseProvidersshouldbeencouragedtoquantifybeappropriatetothelocale,toensurethebestcollaborationandcoordinationofcaretheeconomicbenefitsofpatientcareofpatientsinacost-effectivemanner.betweenpatients,PRprofessionals,andparticipationinPR(e.g.,reductionsinLong-termadherencetohealth-patients’otherhealthcareprovidersarehospitaladmissions)wherepossible.enhancingbehaviors,suchasexercise,crucialtoachievethesegoals.Evidenceofsafetyshouldbeassessedphysicalactivity,abstinencefromsmoking,Recommendationsforensuringqualityofbasedonstandardoperatingpolicies,andimmunization,isakeygoalofPR.PRprogramsareprovidedinBox6.riskassessments,andcriticalincidentAlthoughtheoptimalmeansofmaintainingreporting.PRprogramdirectorsshouldbenefitsachievedinPRisnotfullyclear(85,conductanannualinternalauditofprogram131),PRprofessionals’effortstoassistFutureResearchToAdvanceprocessandoutcomes.PRprogramsshouldpatientsincontinuingtoadheretoexercise,Evidence-basedPolicyinPRalsocollectandrespondtoinformationonincorporatingknowledgegainedinPRintopatientexperience,needs,andsatisfactiondailyliving,andmaintainingcollaborativeAlthoughthescientificrationaleforPRisbefore,during,andafterPR.Qualitystandardsinteractionwithhealthcareprofessionalsestablished,andtheevidenceofthebenefitsBox7:FutureResearchtoAdvanceEvidence-basedPolicyinPRRecommendations:dFurtherresearchshouldbeundertakenregardingthecost-effectivenessofPR:thismayincludeinnovativemodelsofPRdelivery,sitesand/ortimingofPR,PRforrespiratorydisordersotherthanCOPD,andrepeatcoursesofPRovertime.dFurtherinvestigationofalternativemodelsofprovidingPRshouldbeundertakentoimproveaccessanduptake,usingprogrammodelsofknownefficacy.dFurtherinvestigationofalternativemodelsofprovidingPRshouldbeundertakentoaddresstheneedsofpatientswithahighburdenofpsychologicalandmultiplemedicalcomorbidities.dFurtherresearchshouldbedoneregardingbarriersandfacilitatorsofPRprogramreferrals,accessibility,enrollment,andadherenceforpersonswithchronicrespiratorydiseases.dFurtherresearchshouldbeundertakentoassesstheimpactofPRprogramfundingsourceonpatientuseofPR.ActionableItems:dPRexpertsarticulateanddocumentprioritiesforPR-relatedresearchwithinPRassembliesofprofessionalorganizationssuchasATSandERSandcommunicatethemtopatientadvocacygroupsandfundingagenciesviastakeholderforumsandworkshops.dPRexpertslobbyprofessionalsocietiesaswellaspatientadvocacyorganizationsandfederalagenciestodirectcurrentandfuturefundingtowardPRresearch.dHealthcareprofessionalsconductpragmatic,“real-world”trialsofPR.AmericanThoracicSocietyDocuments1381guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSofPRforpersonswithCOPDandotherfeasibilityandsuggestthatclinicalbenefitsmaymorefundingforPRresearchintheseareasformsofchronicrespiratorydiseaseisbeachieved(132–135).Carefullystructuredwillbeneeded.extensiveandconvincing,thereareseveralhome-basedexercisetrainingandMoreinformationisalsoneededareaswhereinfurtherknowledgeisneededrehabilitationthatissupportedbyPRregardingtheclinicalandeconomicbenefitsof(TableE3)(12).Importantly,theTaskForceprogramstaffwithorwithoutspecializedrepeatcoursesofPR(especiallyforpatientsforthisPolicyStatementidentifieskeyareasexerciseequipmentmightbefeasibleinwithchronicrespiratorydisordersotherthanforfutureresearchthatwillsomehealthcareenvironments(136,137).COPD)andregardingoptimalstrategiesforimpactcommissioningpolicyforPRandwillAlternatemethodsforcomponentsofmanagingmedicalandpsychologicalmulti-inturnhavepotentialtoaugmentdeliveryofexercisetraining(suchasuseofelasticmorbidityinthecontextofPR.Also,althoughPRservicesandpatientaccesstoPR.resistancetubesratherthanspecializedtheimpactoffundingsourceonpatientuseofAlthoughthetraditionalmodelsofequipmentforresistancetraining)(138)PRisunclear,sourcesoffundingforPRinpatientandoutpatientPRaresuitableformaybeapplicableacrossabroadrangeofprogramsandreimbursementforpatientmanypatients,alternativemodelsmayalsobesettings.Robustresearchisunderwayinparticipationvarywidely,andthismayinturneffectiveandmayimprovepatientaccess,theseareas(139),andfurtherworkisneededimpactpatientenrollmentandparticipationparticularlyinregionsorhealthcaresystemstovalidatetheseapproaches.Adoptionof(15).YounghealthcareprofessionalswillalsowheretraditionalmodelsofPRarenotfeasible.alternativemodelsforPRwillrequirerequireencouragementandanincreaseinForexample,tele-rehabilitation,whichlinksdemonstrationofcomparableorgreaterinfrastructuretoenablethemtopursueexpertrehabilitationhealthcareproviderswithclinicaloutcomestothoseoftraditionalPRcareersasclinicianinvestigatorswithafocusothersataremotesiteorwithpatientsintheirprograms,aswellasevaluationofsafetyandonPR.Recommendationsforfutureresearchhomes,alsohaspotentialtoimproveaccess.cost-effectiveness,stafftraining,andguidelinetoadvanceevidence-basedpolicyinPRareInitialsmall-scalestudiesdemonstratedevelopment.Thus,tomovethefieldforward,providedinBox7.nThisPolicyStatementwaspreparedbytheATS/ERSTaskForceonPolicyinPulmonaryRehabilitation.Membersofthetaskforceareasfollows:SALLYJ.SINGH,PH.D.AuthorDisclosures:C.L.R.servedonanadvisorycommitteeofGlaxoSmithKline.S.C.L.CAROLYNL.ROCHESTER,M.D.(Co-Chair)RICHARDCASABURI,PH.D.,M.D.servedonanadvisorycommitteeofBoehringerIOANNISVOGIATZIS,PH.D.(Co-Chair)CHRISGARVEY,F.N.P.,M.S.N.,M.P.A.Ingelheim.D.D.M.isaboardmemberoftheRICHARDL.ZUWALLACK,M.D.BARBARAP.YAWN,M.D.,MSC.LungHealthInstituteofCanada.M.A.S.MILOA.PUHAN,M.D.,PH.D.FABIOPITTA,P.T.,PH.D.receivedrelevantfinancialsupportfromCIRO1DARCYD.MARCINIUK,M.D.KYLIEHILL,B.SC.(PHYSIOTHERAPY),PH.D.intheNetherlandsandREVAL/BIOMEDinANNEE.HOLLAND,B.SC.(PHYSIOTHERAPY),PH.D.REBECCACROUCH,P.T.,D.P.T.,M.S.Belgium.M.M.istheNationalClinicalDirectorforRespiratoryServicesforNHSEngland.SUZANNEC.LAREAU,R.N.,M.S.JUDITHGARCIA-AYMERICH,M.D.,PH.D.P.J.W.servedasaspeakerforPhilips/MARTIJNA.SPRUIT,P.T.,PH.D.PETERJ.WIJKSTRA,M.D.,PH.D.Respironics,ResMed,andVIVISOLandANDREWL.RIES,M.D.,M.P.H.SARAHMASEFIELD(ELF)receivedresearchsupportpaidtohis1institutionfromResMed,VIVISOL,andMICHAELMORGAN,M.D.,PH.D.PIPPAPOWELL(ELF)B1VitalAire-AirLiquide.I.V.,A.E.H.,M.A.P.,S.M.,ROGERS.GOLDSTEIN,M.B.CHB.JORNSTAHLBERG,M.D.R.Casaburi,E.M.C.,R.Crouch,J.G.-A.,C.G.,ENRICOM.CLINI,M.D.1TheseindividualsweremembersofthetaskR.S.G.,K.H.,L.N.,F.P.,A.L.R.,S.J.S.,T.T.,LINDANICI,M.D.forcebutwerenotmembersofthewritingB.P.Y.,andR.L.Z.reportednorelevantTHIERRYTROOSTERS,P.T.,PH.D.committee.commercialrelationships.References5.MarciniukDD,BrooksD,ButcherS,DebigareR,DechmanG,FordG,PepinV,ReidD,SheelAW,SticklandMK,etal.Optimizingpulmonary1.SpruitMA,SinghSJ,GarveyC,ZuWallackR,NiciL,RochesterC,HillK,rehabilitationinchronicobstructivepulmonarydisease–practicalHollandAE,LareauSC,ManWD,etal.;ATS/ERSTaskForceonissues:aCanadianThoracicSocietyClinicalPracticeGuideline.CanPulmonaryRehabilitation.AnofficialAmericanThoracicSociety/RespirJ2010;17:159–168.EuropeanRespiratorySocietystatement:keyconceptsandadvancesin6.MarciniukDD,GoodridgeD,HernandezP,RockerG,BalterM,BaileyP,Fordpulmonaryrehabilitation.AmJRespirCritCareMed2013;188:e13–e64.G,BourbeauJ,O’DonnellDE,MaltaisF,etal.Managingdyspneain2.AmericanAssociationofCardiovascularandPulmonaryRehabilitation.patientswithadvancedchronicobstructivepulmonarydisease:aCanadianGuidelinesforcardiacrehabilitationandsecondarypreventionThoracicSocietyClinicalPracticeGuideline.CanRespirJ2011;18:69–78.programs.Champaign,IL,HumanKinetics;7.NiciL,DonnerC,WoutersE,ZuwallackR,AmbrosinoN,BourbeauJ,CaroneM,CelliB,EngelenM,FahyB,etal.;ATS/ERSPulmonary2011.RehabilitationWritingCommittee.AmericanThoracicSociety/3.BoltonCE,Bevan-SmithEF,BlakeyJD,CroweP,ElkinSL,GarrodR,EuropeanRespiratorySocietystatementonpulmonaryrehabilitation.GreeningNJ,HeslopK,HullJH,ManWD,etal.;BritishThoracicSocietyAmJRespirCritCareMed2006;173:1390–1413.PulmonaryRehabilitationGuidelineDevelopmentGroup;BritishThoracic8.O’DonnellDE,AaronS,BourbeauJ,HernandezP,MarciniukDD,BalterSocietyStandardsofCareCommittee.BritishThoracicSocietyguidelineM,FordG,GervaisA,GoldsteinR,HodderR,etal.CanadianThoraciconpulmonaryrehabilitationinadults.Thorax2013;68:ii1–ii30.Societyrecommendationsformanagementofchronicobstructive4.GlobalInitiativeforChronicObstructiveLungDisease(GOLD).Gobalpulmonarydisease:2007update.CanRespirJ2007;14:5B–32B.strategyforthediagnosis,management,andpreventionofCOPD.9.PuhanMA,LareauSC.Evidence-basedoutcomesfrompulmonaryUnitedStates;2014[accessed2015Oct26].Availablefrom:http://rehabilitationinthechronicobstructivepulmonarydiseasepatient.www.goldcopd.org/uploads/users/files/GOLD_Report_2013_Feb20.pdfClinChestMed2014;35:295–301.1382AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTS10.RiesAL,BauldoffGS,CarlinBW,CasaburiR,EmeryCF,MahlerDA,27.TurnerS,EastwoodP,CookA,JenkinsS.ImprovementsinMakeB,RochesterCL,ZuwallackR,HerreriasC.Pulmonarysymptomsandqualityoflifefollowingexercisetraininginolderadultsrehabilitation:jointACCP/AACVPRevidence-basedclinicalpracticewithmoderate/severepersistentasthma.Respiration2011;81:302–310.guidelines.Chest2007;131:4S–42S.28.BradleyJ,MoranF.Physicaltrainingforcysticfibrosis.Cochrane11.RochesterC,FairburnC,CrouchR.PulmonaryrehabilitationforDatabaseSystRev2008;1:CD002768.disordersotherthanchronicobstructivepulmonarydisease.Clin29.CarsonKV,ChandratillekeMG,PicotJ,BrinnMP,EstermanAJ,SmithChestMed2014;35:369–389.BJ.Physicaltrainingforasthma.CochraneDatabaseSystRev2013;12.SinghSJ,ZuWallackRL,GarveyC,SpruitMA;AmericanThoracic9:CD001116.Society/EuropeanRespiratorySocietyTaskForceonPulmonary30.ChanL,ChinLM,KennedyM,WoolstenhulmeJG,NathanSD,Rehabilitation.Learnfromthepastandcreatethefuture:the2013WeinsteinAA,ConnorsG,WeirNA,DrinkardB,LambertiJ,etal.ATS/ERSstatementonpulmonaryrehabilitation.EurRespirJ2013;Benefitsofintensivetreadmillexercisetrainingoncardiorespiratory42:1169–1174.functionandqualityoflifeinpatientswithpulmonaryhypertension.Chest2013;143:333–343.13.JonesSE,GreenSA,ClarkAL,DicksonMJ,NolanAM,MoloneyC,Kon31.deManFS,HandokoML,GroepenhoffH,van’tHulAJ,AbbinkJ,SS,KamalF,GoddenJ,HoweC,etal.PulmonaryrehabilitationKoppersRJ,GrotjohanHP,TwiskJW,BogaardHJ,BoonstraA,etal.followinghospitalisationforacuteexacerbationofCOPD:referrals,Effectsofexercisetraininginpatientswithidiopathicpulmonaryuptakeandadherence.Thorax2014;69:181–182.arterialhypertension.EurRespirJ2009;34:669–675.14.KeatingA,LeeA,HollandAE.Whatpreventspeoplewithchronic32.DowmanL,HillCJ,HollandAE.Pulmonaryrehabilitationforobstructivepulmonarydiseasefromattendingpulmonaryinterstitiallungdisease.CochraneDatabaseSystRev2014;10:rehabilitation?Asystematicreview.ChronRespirDis2011;8:89–99.CD006322.15.SpruitMA,PittaF,GarveyC,ZuWallackRL,RobertsCM,CollinsEG,33.EdvardsenE,SkjønsbergOH,HolmeI,NordslettenL,BorchseniusF,GoldsteinR,McNamaraR,SurpasP,AtsuyoshiK,etal.;ERSAnderssenSA.High-intensitytrainingfollowinglungcancersurgery:RehabilitationandChronicCare,andPhysiotherapistsScientificGroups;arandomisedcontrolledtrial.Thorax2015;70:244–250.AmericanAssociationofCardiovascularandPulmonaryRehabilitation;34.GrangerCL,ChaoC,McDonaldCF,BerneyS,DenehyL.SafetyandATSPulmonaryRehabilitationAssemblyandtheERSCOPDAuditteam.feasibilityofanexerciseinterventionforpatientsfollowinglungDifferencesincontentandorganisationalaspectsofpulmonaryresection:apilotrandomizedcontrolledtrial.IntegrCancerTherrehabilitationprogrammes.EurRespirJ2014;43:1326–1337.2013;12:213–224.16.GloecklR,HalleM,KennK.Intervalversuscontinuoustraininginlung35.Gr¨unigE,LichtblauM,EhlkenN,GhofraniHA,ReichenbergerF,transplantcandidates:arandomizedtrial.JHeartLungTransplantStaehlerG,HalankM,FischerC,SeyfarthHJ,KloseH,etal.Safety2012;31:934–941.andefficacyofexercisetraininginvariousformsofpulmonary17.HollandAE,HillCJ,ConronM,MunroP,McDonaldCF.Shorttermhypertension.EurRespirJ2012;40:84–92.improvementinexercisecapacityandsymptomsfollowingexercise36.HebestreitH,KieserS,JungeS,BallmannM,HebestreitA,Schindlertrainingininterstitiallungdisease.Thorax2008;63:549–554.C,SchenkT,PosseltHG,KriemlerS.Long-termeffectsofapartially18.JonesLW,EvesND,KrausWE,PottiA,CrawfordJ,BlumenthalJA,supervisedconditioningprogrammeincysticfibrosis.EurRespirJPetersonBL,DouglasPS.Thelungcancerexercisetrainingstudy:a2010;35:578–583.randomizedtrialofaerobictraining,resistancetraining,orbothin37.HwangCL,YuCJ,ShihJY,YangPC,WuYT.Effectsofexercisepostsurgicallungcancerpatients:rationaleanddesign.BMCCancertrainingonexercisecapacityinpatientswithnon-smallcelllung2010;10:155.cancerreceivingtargetedtherapy.SupportCareCancer2012;20:19.KlijnPH,OudshoornA,vanderEntCK,vanderNetJ,KimpenJL,3169–3177.HeldersPJ.Effectsofanaerobictraininginchildrenwithcystic38.KriemlerS,KieserS,JungeS,BallmannM,HebestreitA,SchindlerC,fibrosis:arandomizedcontrolledstudy.Chest2004;125:1299–1305.StussiC,HebestreitH.EffectofsupervisedtrainingonFEV1incystic20.MendesFA,GonçalvesRC,NunesMP,Saraiva-RomanholoBM,fibrosis:arandomisedcontrolledtrial.JCystFibros2013;12:CukierA,StelmachR,Jacob-FilhoW,MartinsMA,CarvalhoCR.714–720.Effectsofaerobictrainingonpsychosocialmorbidityandsymptoms39.LangerD,BurtinC,SchepersL,IvanovaA,VerledenG,DecramerM,inpatientswithasthma:arandomizedclinicaltrial.Chest2010;138:TroostersT,GosselinkR.Exercisetrainingafterlungtransplantation331–337.improvesparticipationindailyactivity:arandomizedcontrolledtrial.21.MerelesD,EhlkenN,KreuscherS,GhofraniS,HoeperMM,HalankM,AmJTransplant2012;12:1584–1592.MeyerFJ,KargerG,BussJ,JuengerJ,etal.Exerciseandrespiratory40.LeeAL,HillCJ,CecinsN,JenkinsS,McDonaldCF,BurgeAT,RautelatrainingimproveexercisecapacityandqualityoflifeinpatientswithL,StirlingRG,ThompsonPJ,HollandAE.Theshortandlongtermseverechronicpulmonaryhypertension.Circulation2006;114:effectsofexercisetraininginnon-cysticfibrosisbronchiectasis:a1482–1489.randomisedcontrolledtrial.RespirRes2014;15:44.22.MoorcroftAJ,DoddME,MorrisJ,WebbAK.Individualised41.HaytonC,ClarkA,OliveS,BrowneP,GaleyP,KnightsE,StauntonL,unsupervisedexercisetraininginadultswithcysticfibrosis:JonesA,CoombesE,WilsonAM.Barrierstopulmonarya1yearrandomisedcontrolledtrial.Thorax2004;59:rehabilitation:characteristicsthatpredictpatientattendanceand1074–1080.adherence.RespirMed2013;107:401–407.23.NewallC,StockleyRA,HillSL.Exercisetrainingandinspiratory42.MandalP,SidhuMK,KopeL,PollockW,StevensonLM,PentlandJL,TurnbullK,MacQuarrieS,HillAT.Apilotstudyofpulmonarymuscletraininginpatientswithbronchiectasis.Thorax2005;60:rehabilitationandchestphysiotherapyversuschestphysiotherapy943–948.aloneinbronchiectasis.RespirMed2012;106:1647–1654.24.NishiyamaO,KondohY,KimuraT,KatoK,KataokaK,OgawaT,43.MoranoMT,Ara´ujoAS,NascimentoFB,daSilvaGF,MesquitaR,PintoWatanabeF,ArizonoS,NishimuraK,TaniguchiH.EffectsofJS,deMoraesFilhoMO,PereiraED.Preoperativepulmonarypulmonaryrehabilitationinpatientswithidiopathicpulmonaryrehabilitationversuschestphysicaltherapyinpatientsundergoingfibrosis.Respirology2008;13:394–399.lungcancerresection:apilotrandomizedcontrolledtrial.ArchPhys25.Schneiderman-WalkerJ,PollockSL,CoreyM,WilkesDD,CannyGJ,MedRehabil2013;94:53–58.PedderL,ReismanJJ.Arandomizedcontrolledtrialofa3-year44.OchmannU,Kotschy-LangN,RaabW,KellbergerJ,NowakD,homeexerciseprogramincysticfibrosis.JPediatr2000;136:JorresRA.Long-termefficacyofpulmonaryrehabilitationinpatients304–310.withoccupationalrespiratorydiseases.Respiration2012;84:26.SelvaduraiHC,BlimkieCJ,MeyersN,MellisCM,CooperPJ,Van396–405.AsperenPP.Randomizedcontrolledstudyofin-hospitalexercise45.StefanelliF,MeoliI,CobuccioR,CurcioC,AmoreD,CasazzaD,trainingprogramsinchildrenwithcysticfibrosis.PediatrPulmonolTraceyM,RoccoG.High-intensitytrainingandcardiopulmonary2002;33:194–200.exercisetestinginpatientswithchronicobstructivepulmonaryAmericanThoracicSocietyDocuments1383guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTSdiseaseandnon-small-celllungcancerundergoinglobectomy.EurJSocietystatement:updateonlimbmuscledysfunctioninchronicCardiothoracSurg2013;44:e260–e265.obstructivepulmonarydisease.AmJRespirCritCareMed2014;46.StigtJA,UilSM,vanRiesenSJ,SimonsFJ,DenekampM,ShahinGM,189:e15–e62.GroenHJ.Arandomizedcontrolledtrialofpostthoracotomy64.BredaAP,PereiradeAlbuquerqueAL,JardimC,MorinagaLK,pulmonaryrehabilitationinpatientswithresectablelungcancer.JSuesadaMM,FernandesCJ,DiasB,LourençoRB,SalgeJM,SouzaThoracOncol2013;8:214–221.R.Skeletalmuscleabnormalitiesinpulmonaryarterialhypertension.47.SwigrisJJ,FaircloughDL,MorrisonM,MakeB,KozoraE,BrownKK,PlosOne2014;9:e114101.WamboldtFS.Benefitsofpulmonaryrehabilitationinidiopathic65.MainguyV,MaltaisF,SaeyD,GagnonP,MartelS,SimonM,pulmonaryfibrosis.RespirCare2011;56:783–789.ProvencherS.Peripheralmuscledysfunctioninidiopathicpulmonary48.LeyS,FinkC,RisseF,EhlkenN,FischerC,Ley-ZaporozhanJ,Kauczorarterialhypertension.Thorax2010;65:113–117.HU,KloseH,GruenigE.Magneticresonanceimagingtoassess66.NishiyamaO,TaniguchiH,KondohY,KimuraT,OgawaT,theeffectofexercisetrainingonpulmonaryperfusionandbloodflowWatanabeF,ArizonoS.Quadricepsweaknessisrelatedtoinpatientswithpulmonaryhypertension.EurRadiol2013;23:324–331.exercisecapacityinidiopathicpulmonaryfibrosis.Chest2005;49.MainguyV,MaltaisF,SaeyD,GagnonP,MartelS,SimonM,127:2028–2033.ProvencherS.Effectsofarehabilitationprogramonskeletalmuscle67.OzalpO,Inal-InceD,CalikE,Vardar-YagliN,SaglamM,SavciS,Arikanfunctioninidiopathicpulmonaryarterialhypertension.JCardiopulmH,Bosnak-GucluM,CopluL.ExtrapulmonaryfeaturesofRehabilPrev2010;30:319–323.bronchiectasis:musclefunction,exercisecapacity,fatigue,and50.GarveyC,FullwoodMD,RiglerJ.Pulmonaryrehabilitationexercisehealthstatus.MultidiscipRespirMed2012;7:3.prescriptioninchronicobstructivelungdisease:USsurveyand68.WalshJR,ChambersDC,DavisRJ,MorrisNR,SealeHE,Yerkovichreviewofguidelinesandclinicalpractices.JCardiopulmRehabilPrevST,HopkinsPM.Impairedexercisecapacityafterlung2013;33:314–322.transplantationisrelatedtodelayedrecoveryofmusclestrength.51.DesveauxL,Janaudis-FerreiraT,GoldsteinR,BrooksD.AnClinTransplant2013;27:E504–E511.internationalcomparisonofpulmonaryrehabilitation:asystematic69.WangXN,WilliamsTJ,McKennaMJ,LiJL,FraserSF,SideEA,Snellreview.COPD2015;12:144–153.GI,WaltersEH,CareyMF.Skeletalmuscleoxidativecapacity,fiber52.BajwahS,HigginsonIJ,RossJR,WellsAU,BirringSS,RileyJ,type,andmetabolitesafterlungtransplantation.AmJRespirCritKoffmanJ.ThepalliativecareneedsforfibroticinterstitialCareMed1999;160:57–63.lungdisease:aqualitativestudyofpatients,informal70.L¨oweB,Gr¨afeK,UferC,KroenkeK,Gr¨unigE,HerzogW,BorstMM.caregiversandhealthprofessionals.PalliatMed2013;27:Anxietyanddepressioninpatientswithpulmonaryhypertension.869–876.PsychosomMed2004;66:831–836.53.GuillevinL,ArmstrongI,AldrighettiR,HowardLS,RyfteniusH,Fischer71.Paz-D´ıazH,MontesdeOcaM,L´opezJM,CelliBR.PulmonaryA,LombardiS,StuderS,FerrariP.Understandingtheimpactofrehabilitationimprovesdepression,anxiety,dyspneaandhealthpulmonaryarterialhypertensiononpatients’andcarers’lives.EurstatusinpatientswithCOPD.AmJPhysMedRehabil2007;86:RespirRev2013;22:535–542.30–36.54.HebestreitH,SchmidK,KieserS,JungeS,BallmannM,RothK,72.RyersonCJ,BerkeleyJ,Carrieri-KohlmanVL,PantilatSZ,LandefeldHebestreitA,SchenkT,SchindlerC,PosseltHG,etal.QualityoflifeCS,CollardHR.Depressionandfunctionalstatusarestronglyisassociatedwithphysicalactivityandfitnessincysticfibrosis.BMCassociatedwithdyspneaininterstitiallungdisease.Chest2011;139:PulmMed2014;14:26.609–616.55.MainguyV,ProvencherS,MaltaisF,MalenfantS,SaeyD.Assessment73.WhiteJ,HopkinsRO,GlissmeyerEW,KittermanN,ElliottCG.ofdailylifephysicalactivitiesinpulmonaryarterialhypertension.PlosCognitive,emotional,andqualityoflifeoutcomesinpatientswithOne2011;6:e27993.pulmonaryarterialhypertension.RespirRes2006;7:55.56.MancusoCA,ChoiTN,WestermannH,WenderothS,WellsMT,74.HodgkinJE,FarrellMJ,GibsonSR,KannerRE,KassI,LamptonLM,CharlsonME.ImprovementinasthmaqualityoflifeinpatientsNieldM,PettyTL.AmericanThoracicSociety.Medicalsectionoftheenrolledinaprospectivestudytoincreaselifestylephysicalactivity.AmericanLungAssociation.Pulmonaryrehabilitation.AmRevRespirJAsthma2013;50:103–107.Dis1981;124:663–666.57.MendesFA,LunardiAC,SilvaRA,CukierA,StelmachR,MartinsMA,75.SpruitMA,PenningsHJ,JanssenPP,DoesJD,ScroyenS,AkkermansCarvalhoCR.AssociationbetweenmaximalaerobiccapacityandMA,MostertR,WoutersEF.Extra-pulmonaryfeaturesinCOPDpsychosocialfactorsinadultswithmoderate-to-severeasthma.JpatientsenteringrehabilitationafterstratificationforMRCdyspneaAsthma2013;50:595–599.grade.RespirMed2007;101:2454–2463.58.MiyamotoS,NagayaN,SatohT,KyotaniS,SakamakiF,FujitaM,76.PuhanMA,Gimeno-SantosE,ScharplatzM,TroostersT,WaltersEH,NakanishiN,MiyatakeK.ClinicalcorrelatesandprognosticSteurerJ.Pulmonaryrehabilitationfollowingexacerbationsofsignificanceofsix-minutewalktestinpatientswithchronicobstructivepulmonarydisease.CochraneDatabaseSystprimarypulmonaryhypertension:comparisonwithRev2011;10:CD005305.cardiopulmonaryexercisetesting.AmJRespirCritCareMed77.CrinerGJ,BourbeauJ,DiekemperRL,OuelletteDR,GoodridgeD,2000;161:487–492.HernandezP,CurrenK,BalterMS,BhutaniM,CampPG,etal.59.MyrdalG,ValtysdottirS,LambeM,StahleE.Qualityoflifefollowing˚Preventionofacuteexacerbationsofchronicobstructivepulmonarylungcancersurgery.Thorax2003;58:194–197.disease:AmericanCollegeofChestPhysiciansandCanadian60.NovoaN,VarelaG,Jim´enezMF,ArandaJL.InfluenceofmajorThoracicSocietyguideline.Chest2015;147:894–942.pulmonaryresectiononpostoperativedailyambulatoryactivityofthe78.CliniE,FoglioK,BianchiL,PortaR,VitaccaM,AmbrosinoN.In-patients.InteractCardiovascThoracSurg2009;9:934–938.hospitalshort-termtrainingprogramforpatientswithchronicairway61.OstroffJS,KrebsP,CoupsEJ,BurkhalterJE,FeinsteinMB,Steingartobstruction.Chest2001;120:1500–1505.RM,LogueAE,ParkBJ.Health-relatedqualityoflifeamongearly-79.WoottonSL,NgLW,McKeoughZJ,JenkinsS,HillK,EastwoodPR,stage,non-smallcell,lungcancersurvivors.LungCancer2011;71:HillmanDR,CecinsN,SpencerLM,JenkinsC,etal.Ground-based103–108.walkingtrainingimprovesqualityoflifeandexercisecapacityin62.TroostersT,LangerD,VrijsenB,SegersJ,WoutersK,JanssensW,COPD.EurRespirJ2014;44:885–894.GosselinkR,DecramerM,DupontL.Skeletalmuscleweakness,80.BeauchampMK,Janaudis-FerreiraT,GoldsteinRS,BrooksD.Optimalexercisetoleranceandphysicalactivityinadultswithcysticfibrosis.durationofpulmonaryrehabilitationforindividualswithchronicEurRespirJ2009;33:99–106.obstructivepulmonarydisease:asystematicreview.ChronRespir63.MaltaisF,DecramerM,CasaburiR,BarreiroE,BurelleY,Debigar´eR,Dis2011;8:129–140.DekhuijzenPN,FranssenF,Gayan-RamirezG,GeaJ,etal.;ATS/81.TroostersT,CasaburiR,GosselinkR,DecramerM.PulmonaryERSAdHocCommitteeonLimbMuscleDysfunctioninCOPD.rehabilitationinchronicobstructivepulmonarydisease.AmJRespirAnofficialAmericanThoracicSociety/EuropeanRespiratoryCritCareMed2005;172:19–38.1384AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTS82.FoglioK,BianchiL,AmbrosinoN.Isitreallyusefultorepeatoutpatient100.BrooksD,SottanaR,BellB,HannaM,LaframboiseL,SelvanayagarajahpulmonaryrehabilitationprogramsinpatientswithchronicairwayS,GoldsteinR.Characterizationofpulmonaryrehabilitationprogramsobstruction?A2-yearcontrolledstudy.Chest2001;119:1696–1704.inCanadain2005.CanRespirJ2007;14:87–92.83.MeisJJ,BosmaCB,SpruitMA,FranssenFM,JanssenDJ,TeixeiraPJ,101.CollinsEG,BauldoffG,CarlinB,CrouchR,EmeryCF,GarveyC,AugustinIM,WoutersEF,deVriesNK,ScholsAM,etal.AqualitativeHillingL,LimbergT,ZuWallackR,NiciL;AmericanAssociationofassessmentofCOPDpatients’experiencesofpulmonaryCardiovascularandPulmonaryRehabilitation.Clinicalcompetencyrehabilitationandguidancebyhealthcareprofessionals.RespirMedguidelinesforpulmonaryrehabilitationprofessionals:position2014;108:500–510.statementoftheAmericanAssociationofCardiovascularand84.ZwerinkM,Brusse-KeizerM,vanderValkPD,ZielhuisGA,MonninkhofPulmonaryRehabilitation.JCardiopulmRehabilPrev2014;34:EM,vanderPalenJ,FrithPA,EffingT.Selfmanagementforpatients291–302.withchronicobstructivepulmonarydisease.CochraneDatabase102.RochesterCL,SpanevelloA.HeterogeneityofpulmonarySystRev2014;3:CD002990.rehabilitation:likeapplesandoranges-bothhealthyfruit.Eur85.SpencerLM,AlisonJA,McKeoughZJ.MaintainingbenefitsfollowingRespirJ2014;43:1223–1226.pulmonaryrehabilitation:arandomisedcontrolledtrial.EurRespirJ103.SabitR,GriffithsTL,WatkinsAJ,EvansW,BoltonCE,ShaleDJ,Lewis2010;35:571–577.KE.Predictorsofpoorattendanceatanoutpatientpulmonary86.JohnstonKN,YoungM,GrimmerKA,AnticR,FrithPA.Barriersto,andrehabilitationprogramme.RespirMed2008;102:819–824.facilitatorsfor,referraltopulmonaryrehabilitationinCOPDpatients104.ArbaneG,TropmanD,JacksonD,GarrodR.EvaluationofanearlyfromtheperspectiveofAustraliangeneralpractitioners:aqualitativeexerciseinterventionafterthoracotomyfornon-smallcelllungstudy.PrimCareRespirJ2013;22:319–324.cancer(NSCLC),effectsonqualityoflife,musclestrengthand87.JointRoyalCollegesofPhysicianTrainingBoard.2010Respiratoryexercisetolerance:randomisedcontrolledtrial.LungCancer2011;medicinesingleCCTdecisionaid[accessed2015Oct26].Available71:229–234.from:http://www.jrcptb.org.uk/documents/2010-respiratory-105.ChinRC,GuenetteJA,ChengS,RaghavanN,Amornputtisathapornmedicine-single-cct-decision-aid-revised-2014N,Cort´es-T´ellesA,WebbKA,O’DonnellDE.Doesthe88.AccreditationCouncilforGraduateMedicalEducation.Programrespiratorysystemlimitexerciseinmildchronicobstructiverequirementsforgraduatemedicaleducationinpulmonarydiseaseandpulmonarydisease?AmJRespirCritCareMed2013;187:1315–1323.criticalcaremedicine(internalmedicine).2014[accessed2015Oct26].Availablefrom:https://www.acgme.org/acgmeweb/portals/0/pfassets/106.GuenetteJA,JensenD,WebbKA,OfirD,RaghavanN,O’DonnellDE.2013-pr-faq-pif/156_pulmonary_critical_care_int_med_07132013.pdfSexdifferencesinexertionaldyspneainpatientswithmildCOPD:physiologicalmechanisms.RespirPhysiolNeurobiol2011;177:89.RoyalCollegeofPhysiciansandSurgeonsofCanada.Objectivesof218–227.traininginthesubspecialtyofadultrespirology.2011[accessed2015Oct26].Availablefrom:https://www.medicine.mcgill.ca/107.O’DonnellDE,LavenezianaP,WebbK,NederJA.Chronicobstructivepulmonarydisease:clinicalintegrativephysiology.ClinChestMedpostgrad/accreditation_2013/PSQs/2_Respirology_adult/2014;35:51–69.05_OTR_Respirology_adult_2011.pdf108.OfirD,LavenezianaP,WebbKA,LamYM,O’DonnellDE.90.Besluitlongziektenentuberculose1-januari-2013(pdf)[accessed2015MechanismsofdyspneaduringcycleexerciseinsymptomaticOct26].Availablefrom:http://knmg.artsennet.nl/Opleiding-en-patientswithGOLDstageIchronicobstructivepulmonarydisease.herregistratie/CGS/Regelgeving/Huidige-regelgeving/Longziekten-en-AmJRespirCritCareMed2008;177:622–629.tuberculose.htm109.Orozco-LeviM,CoronellC,Ram´ırez-SarmientoA,LloretaJ,Mart´ınez-91.Curricula[accessed2015Oct26].Availablefrom:https://LlorensJ,GaldizJB,GeaJ.Injuryofperipheralmusclesinsmokersmembers.racp.edu.au/page/advanced-curriculawithchronicobstructivepulmonarydisease.UltrastructPathol92.Recommendationsforthediagnosisandtreatmentofchronic2012;36:228–238.obstructivepulmonarydisease(COPD),April2011[inSpanish]110.FastenauA,vanSchayckOC,GosselinkR,AretzKC,MurisJW.[accessed2015Oct26].Availablefrom:https://www.alatorax.org/Discrepancybetweenfunctionalexercisecapacityanddailyepoc/guia-epoc-alat/recomendaciones-para-el-diagnostico-y-physicalactivity:across-sectionalstudyinpatientswithmildtotratamiento-de-la-enfermedad-pulmonar-obstructiva-cronica-epoc-moderateCOPD.PrimCareRespirJ2013;22:425–430.abril-2011111.VanRemoortelH,HornikxM,DemeyerH,LangerD,BurtinC,93.BTS.IMPRESSguidetopulmonaryrehabilitation.2011[accessedDecramerM,GosselinkR,JanssensW,TroostersT.Dailyphysical2015Oct26].Availablefrom:http://www.Impressresp.Com/activityinsubjectswithnewlydiagnosedCOPD.Thorax2013;68:index.Php?Option=com_content&view=article&id=38:Pulmonary-962–963.rehabilitation&catid=17:Service-delivery&itemid=32112.HayashiY,SenjyuH,IguchiA,IwaiS,KanadaR,HondaS,OzawaH.94.GriffithsTL,BurrML,CampbellIA,Lewis-JenkinsV,MullinsJ,ShielsK,PrevalenceofdepressivesymptomsinJapanesemalepatientswithTurner-LawlorPJ,PayneN,NewcombeRG,IonescuAA,etal.Resultschronicobstructivepulmonarydisease.PsychiatryClinNeurosciat1yearofoutpatientmultidisciplinarypulmonaryrehabilitation:a2011;65:82–88.randomisedcontrolledtrial.Lancet2000;355:362–368.113.SinDD,WuL,ManSF.Therelationshipbetweenreducedlung95.GriffithsTL,PhillipsCJ,DaviesS,BurrML,CampbellIA.Costfunctionandcardiovascularmortality:apopulation-basedstudyeffectivenessofanoutpatientmultidisciplinarypulmonaryandasystematicreviewoftheliterature.Chest2005;127:rehabilitationprogramme.Thorax2001;56:779–784.1952–1959.96.ZoumotZ,JordanS,HopkinsonNS.Emphysema:timetosayfarewell114.HurstJR,VestboJ,AnzuetoA,LocantoreN,M¨ullerovaH,Tal-Singertotherapeuticnihilism.Thorax2014;69:973–975.R,MillerB,LomasDA,AgustiA,MacneeW,etal.;Evaluationof97.BTS.IMPRESSguidetotherelativevalueofCOPDinterventions:COPDLongitudinallytoIdentifyPredictiveSurrogateEndpointsexecutivesummary.2012[accessed2015Oct26].Availablefrom:(ECLIPSE)Investigators.Susceptibilitytoexacerbationinchronichttp://www.Impressresp.Com/index.Php?Option=com_docman&task=obstructivepulmonarydisease.NEnglJMed2010;363:doc_view&gid=52&itemid=821128–1138.98.CaliforniaPulmonaryRehabilitationCollaborativeGroup.Effectsof115.Garc´ıa-RioF,SorianoJB,MiravitllesM,MuñozL,Duran-TauleriaE,pulmonaryrehabilitationondyspnea,qualityoflife,andhealthcareS´anchezG,SobradilloV,AncocheaJ.OverdiagnosingsubjectscostsinCalifornia.JCardiopulmRehabil2004;24:52–62.withCOPDusingthe0.7fixedratio:correlationwithapoorhealth-99.RaskinJ,SpieglerP,McCuskerC,ZuWallackR,BernsteinM,BusbyJ,relatedqualityoflife.Chest2011;139:1072–1080.DiLauroP,GriffithsK,HaggertyM,HoveyL,etal.Theeffectof116.CheeA,SinDD.Treatmentofmildchronicobstructivepulmonarypulmonaryrehabilitationonhealthcareutilizationinchronicdisease.IntJChronObstructPulmonDis2008;3:563–573.obstructivepulmonarydisease:theNortheastPulmonary117.J´acomeC,MarquesA.PulmonaryrehabilitationformildCOPD:aRehabilitationConsortium.JCardiopulmRehabil2006;26:231–236.systematicreview.RespirCare2014;59:588–594.AmericanThoracicSocietyDocuments1385guide.medlive.cn
AMERICANTHORACICSOCIETYDOCUMENTS118.VogiatzisI,TerzisG,StratakosG,CherouveimE,AthanasopoulosD,multidimensionalprofiling.EurRespirJ[onlineaheadofprint]9OctSpetsiotiS,NasisI,MantaP,RoussosC,ZakynthinosS.Effectof2015;DOI:10.1183/13993003.00350-2015.pulmonaryrehabilitationonperipheralmusclefiberremodelingin131.RingbaekT,BrondumE,MartinezG,ThogersenJ,LangeP.Long-patientswithCOPDinGOLDstagesIItoIV.Chest2011;140:termeffectsof1-yearmaintenancetrainingonphysicalfunctioning744–752.andhealthstatusinpatientswithCOPD:arandomizedcontrolled119.RiesAL,KaplanRM,LimbergTM,PrewittLM.Effectsofpulmonarystudy.JCardiopulmRehabilPrev2010;30:47–52.rehabilitationonphysiologicandpsychosocialoutcomesin132.HollandAE,HillCJ,RochfordP,FioreJ,BerlowitzDJ,McDonaldCF.patientswithchronicobstructivepulmonarydisease.AnnInternTelerehabilitationforpeoplewithchronicobstructivepulmonaryMed1995;122:823–832.disease:feasibilityofasimple,realtimemodelofsupervised120.SeymourJM,MooreL,JolleyCJ,WardK,CreaseyJ,SteierJS,YungB,exercisetraining.JTelemedTelecare2013;19:222–226.ManWD,HartN,PolkeyMI,etal.Outpatientpulmonaryrehabilitation133.SticklandM,JourdainT,WongEY,RodgersWM,JendzjowskyNG,followingacuteexacerbationsofCOPD.Thorax2010;65:423–428.MacdonaldGF.UsingTelehealthtechnologytodeliverpulmonary121.CoteCG,DordellyLJ,CelliBR.ImpactofCOPDexacerbationsonrehabilitationinchronicobstructivepulmonarydiseasepatients.patient-centeredoutcomes.Chest2007;131:696–704.CanRespirJ2011;18:216–220.122.KesslerR,StahlE,VogelmeierC,HaughneyJ,TrudeauE,L¨˚ofdahlCG,134.TousignantM,MarquisN,Pag´eC,ImukuzeN,M´etivierA,St-OngeV,PartridgeMR.Patientunderstanding,detection,andexperienceofTremblayA.In-hometelerehabilitationforolderpersonswithCOPDexacerbations:anobservational,interview-basedstudy.chronicobstructivepulmonarydisease:apilotstudy.IntJChest2006;130:133–142.Telerehabil2012;4:7–14.123.PittaF,TroostersT,ProbstVS,SpruitMA,DecramerM,GosselinkR.135.GoldsteinRS,O’HoskiS.TelemedicineinCOPD:timetopause.ChestPhysicalactivityandhospitalizationforexacerbationofCOPD.2014;145:945–949.Chest2006;129:536–544.136.MaltaisF,BourbeauJ,ShapiroS,LacasseY,PerraultH,BaltzanM,124.Demenzhandbuch[accessed2015Oct26].Availablefrom:https://HernandezP,RouleauM,JulienM,ParenteauS,etal.;Chronicstatic.uni-graz.at/fileadmin/Unikid-Unicare/Broschueren/ObstructivePulmonaryDiseaseAxisofRespiratoryHealthNetwork,Demenzhandbuch.pdfFondsderechercheensant´eduQu´ebec.Effectsofhome-based125.AustralianLungFoundation.PulmonaryRehabilitationToolkitpulmonaryrehabilitationinpatientswithchronicobstructivepulmonary[accessed2015Oct26].Availablefrom:http://www.disease:arandomizedtrial.AnnInternMed2008;149:869–878.pulmonaryrehab.com.au/welcome.asp137.PradellaCO,BelmonteGM,MaiaMN,DelgadoCS,LuiseAP,126.JenkinsS,HillK,CecinsNM.Stateoftheart:howtosetupapulmonaryNascimentoOA,GazzottiMR,JardimJR.Home-basedpulmonaryrehabilitationprogram.Respirology2010;15:1157–1173.rehabilitationforsubjectswithCOPD:arandomizedstudy.Respir127.GarberCE,BlissmerB,DeschenesMR,FranklinBA,LamonteMJ,LeeCare2015;60:526–532.IM,NiemanDC,SwainDP;AmericanCollegeofSportsMedicine.AmericanCollegeofSportsMedicinepositionstand.Quantityand138.RamosEM,deToledo-ArrudaAC,FoscoLC,BonfimR,BertoliniGN,qualityofexercisefordevelopingandmaintainingcardiorespiratory,GuarnierFA,CecchiniR,PastreCM,LangerD,GosselinkR,etal.musculoskeletal,andneuromotorfitnessinapparentlyhealthyTheeffectsofelastictubing-basedresistancetrainingcomparedadults:guidanceforprescribingexercise.MedSciSportsExercwithconventionalresistancetraininginpatientswithmoderate2011;43:1334–1359.chronicobstructivepulmonarydisease:arandomizedclinicaltrial.128.AmericanCollegeofSportsMedicine.ACSM’sguidelinesforexerciseClinRehabil2014;28:1096–1106.testingandprescription.Philadelphia,PA:LippincottWilliams&139.ClinicalTrials.gov[accessed2015Oct26].Availablefrom:https://Wilkins;2013.clinicaltrials.gov/ct2/show/NCT01423227129.WatzH,PittaF,RochesterCL,Garcia-AymerichJ,ZuWallackR,140.LacasseY,GoldsteinR,LassersonTJ,MartinS.PulmonaryTroostersT,VaesAW,PuhanMA,JehnM,PolkeyMI,etal.Anrehabilitationforchronicobstructivepulmonarydisease.CochraneofficialEuropeanRespiratorySocietystatementonphysicalactivityDatabaseSystRev2006;4:CD003793.inCOPD.EurRespirJ2014;44:1521–1537.141.LavioletteL,BourbeauJ,BernardS,LacasseY,PepinV,BretonMJ,130.SpruitMA,AugustinIM,VanfleterenL,JanssenDJ,GaffronS,BaltzanM,RouleauM,MaltaisF.AssessingtheimpactofPenningsHJ,SmeenkF,PietersW,vandenBerghJJ,MichelsAJ,pulmonaryrehabilitationonfunctionalstatusinCOPD.Thoraxetal.DifferentialresponsetopulmonaryrehabilitationinCOPD:2008;63:115–121.1386AmericanJournalofRespiratoryandCriticalCareMedicineVolume192Number11|December12015guide.medlive.cn